The human body possesses remarkable healing capabilities, yet the persistent problem of fibrosis has long baffled medical researchers. Unlike typical wound healing where damaged tissue is replaced with functional cells, fibrosis results in thick, collagen-rich scar tissue that often impairs organ function. Recent breakthroughs in regenerative medicine, however, are revealing the biological code that may allow us to reverse this process.
The Fibrosis Conundrum
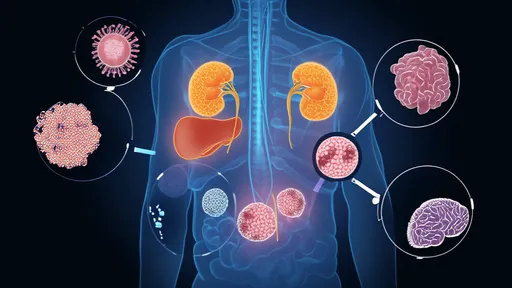
Fibrosis occurs when the body's repair mechanisms go awry, creating excessive extracellular matrix deposits instead of restoring original tissue architecture. This pathological scarring affects nearly every major organ system—from liver cirrhosis and pulmonary fibrosis to cardiac scarring post-heart attack. The consequences are often devastating, with fibrotic diseases accounting for up to 45% of deaths in the developed world according to some estimates.
What makes fibrosis particularly insidious is its self-perpetuating nature. Once initiated, the process creates a feedback loop where myofibroblasts—the primary collagen-producing cells—continue their activity even after the initial injury has healed. Traditional treatments have focused on slowing progression rather than achieving true reversal, leaving millions of patients with limited therapeutic options.
Cellular Alchemy: Reprogramming Scar Tissue
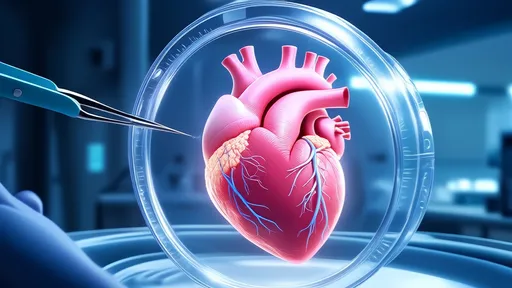
Groundbreaking research published in Nature last year demonstrated that specific molecular signals could convert myofibroblasts back into functional tissue cells in mouse models of heart fibrosis. The key lies in manipulating the Hippo signaling pathway, a conserved biological circuit that controls organ size and regeneration across species.
When researchers inhibited this pathway in fibrotic mouse hearts, they observed something extraordinary: scar tissue began dissolving as myofibroblasts transformed into cardiomyocyte-like cells. The treated hearts showed improved contraction and electrical conduction—functions typically lost to scarring. This cellular reprogramming approach represents a paradigm shift from merely halting fibrosis to actively reversing it.
The Liver's Remarkable Plasticity
Perhaps the most promising developments come from hepatic research. The liver possesses an innate capacity for regeneration unmatched by other solid organs. Scientists at the University of California recently identified a population of "hybrid hepatocytes" that naturally resist fibrosis while maintaining regenerative potential. These cells appear to hold the blueprint for scar-free healing.
By isolating the genetic signatures of these resilient cells, researchers have begun developing targeted therapies that mimic their behavior. Early clinical trials using modified RNA sequences to reprogram fibrotic liver cells have shown unprecedented success in reducing collagen deposits while restoring metabolic function. Patients who received these experimental treatments exhibited measurable improvements in liver elasticity—a direct indicator of fibrosis reversal.
Breaking the Extracellular Matrix Code
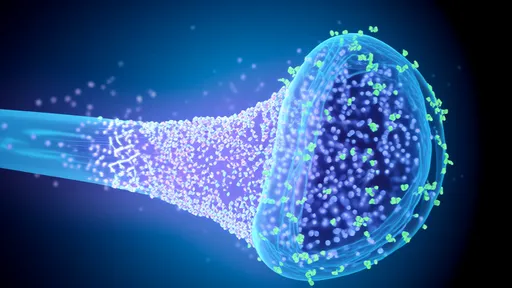
The extracellular matrix (ECM)—long considered a static scaffold—is now understood to be a dynamic information network. Matrix metalloproteinases (MMPs), enzymes that degrade ECM components, have emerged as crucial players in fibrosis reversal. However, their activity must be precisely timed and localized; unchecked MMP activity can cause tissue destruction rather than remodeling.
Innovative drug delivery systems using nanotechnology now allow for spatiotemporal control of these enzymes. Researchers have designed "smart" nanoparticles that release MMP activators only when they encounter specific pH levels or mechanical pressures characteristic of fibrotic tissue. This targeted approach has shown particular promise in pancreatic fibrosis models, where conventional therapies often fail.
Epigenetic Erasers: Rewriting the Scar Memory
Perhaps the most revolutionary insight comes from epigenetics—the study of how environmental factors influence gene expression without altering DNA sequences. Fibrotic cells appear to maintain a "memory" of their pathological state through specific histone modifications and DNA methylation patterns.
Experimental compounds that modify these epigenetic marks have achieved what was previously unthinkable: convincing mature scar tissue to revert to a more plastic, regenerative state. In one striking example, a combination of histone deacetylase inhibitors and DNA methyltransferase inhibitors enabled partial regrowth of functional alveoli in end-stage pulmonary fibrosis models. The implications for chronic lung disease patients are profound.
Challenges on the Path to Clinical Translation
While these scientific advances are exhilarating, significant hurdles remain before fibrosis reversal becomes routine clinical practice. The complexity of biological systems means that interventions successful in one organ may prove ineffective or even harmful in another. Moreover, the very mechanisms that enable fibrosis reversal—such as cellular reprogramming—could theoretically increase cancer risk if not properly controlled.
Researchers emphasize the need for sophisticated delivery methods that can target specific cell populations while sparing others. Combination therapies addressing multiple aspects of the fibrotic process simultaneously may offer the best chance for meaningful clinical outcomes. Several such multimodal approaches are currently in phase II trials for kidney and dermal fibrosis.
A New Era of Regenerative Medicine
The emerging science of fibrosis reversal represents more than just another medical advance—it challenges our fundamental understanding of cellular identity and tissue plasticity. As we decipher the biological code that governs scar formation and resolution, we edge closer to therapies that could potentially restore damaged organs to full function.
For millions living with fibrotic diseases, these developments herald a future where "irreversible" damage may become treatable. The scars that once marked permanent injury could one day be mere waypoints in the body's ongoing journey of renewal—a testament to medicine's growing ability to collaborate with the body's innate wisdom rather than simply combat its pathologies.

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025