In the ever-evolving landscape of medical science, mitochondrial transplantation has emerged as a groundbreaking approach to rejuvenating failing cells. This innovative technique, still in its experimental stages, holds the promise of addressing a myriad of degenerative diseases by replacing damaged mitochondria with healthy ones. The implications are vast, ranging from treating heart disease to neurodegenerative disorders, offering a glimmer of hope where traditional therapies have fallen short.
The concept of mitochondrial transplantation revolves around the idea that these tiny powerhouses of the cell, when compromised, can be replaced or supplemented to restore cellular function. Mitochondria are responsible for producing adenosine triphosphate (ATP), the energy currency of the cell. When they malfunction, cells struggle to perform even the most basic functions, leading to tissue deterioration and organ failure. By introducing healthy mitochondria into these ailing cells, scientists aim to reverse or mitigate the damage.
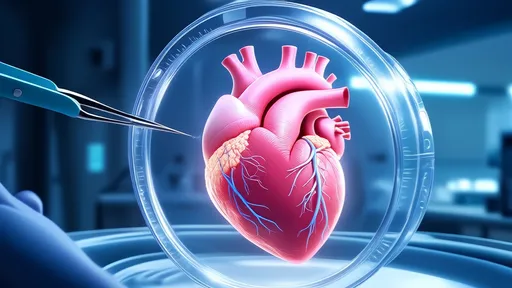
Recent studies have demonstrated the potential of this technique in cardiac care. Patients suffering from myocardial ischemia, a condition where heart tissue is starved of oxygen, have shown remarkable improvement following mitochondrial transplants. In one clinical trial, surgeons extracted mitochondria from a patient’s own skeletal muscle and injected them directly into the affected heart tissue. The results were nothing short of astonishing—improved heart function, reduced scar tissue, and enhanced recovery rates.
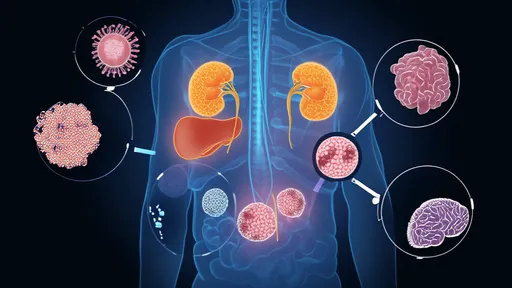
But the applications don’t end there. Neurodegenerative diseases like Parkinson’s and Alzheimer’s, which are characterized by the progressive death of neurons, could also benefit from mitochondrial transplantation. Researchers hypothesize that replacing damaged mitochondria in neurons could slow or even halt the progression of these debilitating conditions. Early experiments in animal models have yielded encouraging results, with treated subjects showing significant improvements in motor function and cognitive performance.
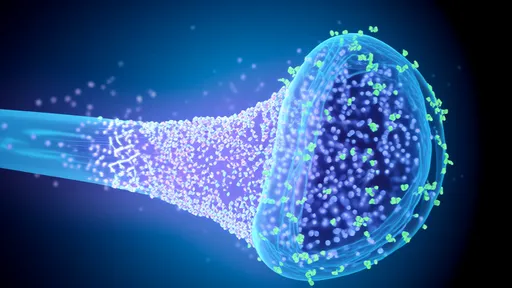
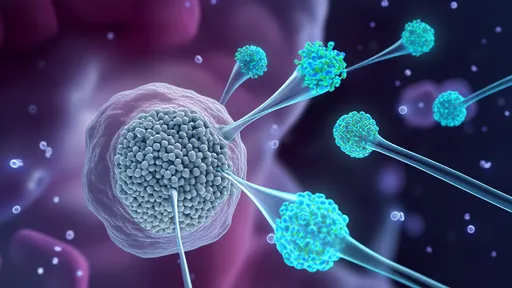
The process of mitochondrial transplantation is as fascinating as it is complex. Scientists must first isolate healthy mitochondria from donor cells, a task that requires precision and care. These mitochondria are then delivered to the target cells using various methods, including direct injection, viral vectors, or even nanotechnology. Each approach has its own set of challenges and advantages, and researchers are continually refining these techniques to improve efficacy and safety.
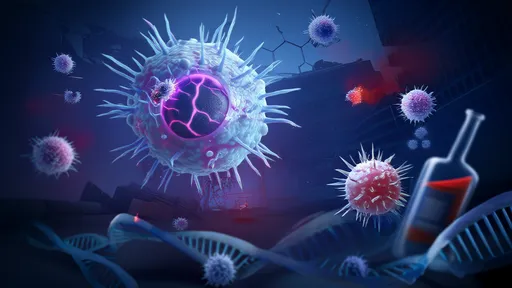
One of the most significant hurdles facing mitochondrial transplantation is the risk of immune rejection. While using a patient’s own mitochondria minimizes this risk, it isn’t always feasible, especially in cases where the patient’s mitochondria are universally compromised. Scientists are exploring ways to engineer universal donor mitochondria that can evade the immune system, a development that could revolutionize the field.
Ethical considerations also loom large. As with any emerging medical technology, mitochondrial transplantation raises questions about accessibility, long-term effects, and the potential for misuse. Should this therapy become widely available, it could exacerbate existing healthcare disparities, with only the wealthiest patients able to afford it. Moreover, the long-term consequences of introducing foreign mitochondria into the body are still unknown, necessitating rigorous oversight and continued research.
Despite these challenges, the future of mitochondrial transplantation looks promising. Researchers are optimistic that with continued investment and innovation, this technique could become a standard treatment for a host of currently incurable diseases. The ability to breathe new life into failing cells represents a paradigm shift in medicine, one that could redefine our approach to aging and degeneration.
In the coming years, as clinical trials expand and technologies advance, mitochondrial transplantation may well transition from the realm of experimental science to mainstream medicine. For patients with few other options, this could mean the difference between a life of decline and one of renewed vitality. The journey is just beginning, but the potential is limitless.

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025