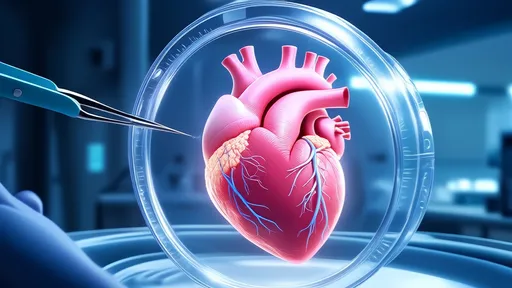
In a groundbreaking medical milestone, the field of xenotransplantation has taken a revolutionary leap forward with the successful transplantation of a genetically modified pig heart into a human patient. This unprecedented achievement marks a turning point in addressing the critical shortage of donor organs and opens new avenues for saving countless lives. The procedure, performed by a team of pioneering surgeons, demonstrates the potential of CRISPR gene-editing technology to overcome biological barriers that have long hindered cross-species organ transplantation.
The recipient, a 57-year-old man with terminal heart disease, had exhausted all conventional treatment options and was deemed ineligible for a traditional human heart transplant. With no alternatives left, the medical team received emergency authorization from the U.S. Food and Drug Administration to attempt the experimental procedure. The genetically engineered pig heart underwent extensive modifications to reduce the risk of rejection, including the knockout of specific pig genes and the insertion of human genes to improve compatibility.
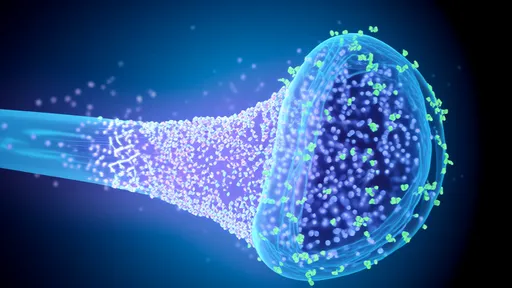
What makes this achievement particularly remarkable is the complex series of genetic alterations made to the donor pig. Scientists disabled four porcine genes that trigger aggressive human immune responses and added six human genes to promote acceptance of the organ. Additionally, they inactivated retroviruses inherent in pig DNA that could potentially infect human cells. These modifications represent years of meticulous research into the molecular mechanisms of organ rejection and cross-species viral transmission.
The surgical team faced numerous challenges during the operation, not least of which was ensuring the pig heart could function properly in the human circulatory system. Pig hearts differ anatomically from human hearts, with variations in chamber size, valve structure, and electrical conduction pathways. The surgeons had to make precise adjustments to accommodate these differences while maintaining proper blood flow and rhythm. Post-operative monitoring revealed that the heart adapted surprisingly well to its new environment, maintaining stable circulation without immediate signs of rejection.
Ethical considerations surrounding xenotransplantation have been at the forefront of discussions within the medical community. Critics have raised concerns about animal welfare, the potential for creating new zoonotic diseases, and the psychological impact on patients receiving animal organs. However, proponents argue that the potential to save human lives justifies the research, especially given the staggering statistics: in the United States alone, seventeen people die each day waiting for an organ transplant. The successful pig heart transplant offers hope that xenotransplantation could eventually eliminate organ waiting lists altogether.
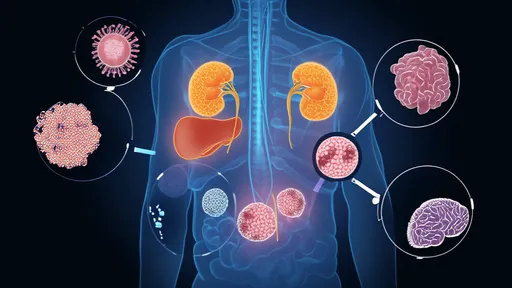
Beyond the immediate medical implications, this breakthrough has sparked important conversations about the future of organ transplantation. Researchers are now exploring whether similar genetic engineering techniques could be applied to other organs like kidneys, livers, and lungs. The possibility of creating "universal donor" pigs—animals whose organs could be transplanted into any human recipient without extensive genetic matching—could transform transplant medicine. Such developments would dramatically reduce waiting times and make transplants accessible to patients who currently have no hope of receiving a human organ.
The patient's recovery process is being closely monitored by a multidisciplinary team of specialists. Initial results show promising signs of organ function, though the long-term outcomes remain uncertain. The medical team is particularly vigilant for signs of organ rejection, infection, or unforeseen complications arising from the interspecies transfer. Immunosuppressive drugs, specially tailored for this unique situation, are being administered to prevent rejection while minimizing side effects. Each day the heart continues to function normally provides valuable data that will shape future xenotransplantation attempts.
This achievement builds upon decades of research in xenotransplantation. Previous attempts at cross-species organ transplants, including baboon-to-human heart transplants in the 1980s, ultimately failed due to immune rejection. The critical difference this time lies in the precision of genetic engineering. CRISPR technology allows scientists to make targeted modifications to the pig genome that were impossible with earlier techniques. This level of control over the donor organ's biological characteristics represents a quantum leap in transplantation science.
Looking ahead, researchers caution that widespread clinical application of pig organ transplants remains years away. While this case demonstrates the feasibility of the approach, numerous hurdles must still be overcome. Long-term studies are needed to assess organ durability, the risk of late-onset rejection, and potential complications that might emerge over time. Regulatory frameworks will need to be developed to govern the breeding of genetically modified animals and the approval process for xenotransplantation procedures. Additionally, the cost of these highly engineered organs must be addressed to ensure equitable access.
The successful pig heart transplant has ignited both excitement and debate within the scientific community and beyond. Some hail it as the beginning of a new era in medicine, while others urge caution regarding the ethical and safety implications. What remains undeniable is that this achievement represents a remarkable convergence of genetic engineering, surgical innovation, and medical courage. As research progresses, the dream of an unlimited supply of transplantable organs may soon transition from science fiction to medical reality, fundamentally changing how we approach end-stage organ failure.
Public reaction to the news has been mixed, with many expressing awe at the scientific achievement while others voice discomfort with the idea of animal-to-human organ transfers. Religious leaders have begun weighing in on the theological implications, with some denominations embracing the technology as an example of human ingenuity serving divine purpose, while others question the morality of manipulating animal genomes for human benefit. These discussions highlight how medical breakthroughs often force society to confront complex questions at the intersection of science, ethics, and belief systems.
From a technical perspective, the procedure's success validates years of incremental advances across multiple scientific disciplines. Immunologists made crucial discoveries about immune system triggers in xenotransplantation. Geneticists developed increasingly sophisticated gene-editing tools. Surgeons refined techniques for organ preservation and transplantation. This interdisciplinary collaboration serves as a model for how complex medical challenges can be addressed through coordinated research efforts. The knowledge gained from this case will undoubtedly accelerate progress in related fields, potentially benefiting patients with conditions beyond just organ failure.
As the medical community processes this landmark event, attention is turning to the next steps in xenotransplantation research. Several biotechnology companies are racing to develop standardized lines of gene-edited pigs optimized for organ donation. Clinical trials involving multiple patients will be necessary to establish safety and efficacy benchmarks. Meanwhile, researchers continue working on complementary technologies like organ perfusion systems that could keep donor organs viable for longer periods, further increasing the potential success of transplants.
The economic implications of successful xenotransplantation could be profound. The global organ transplant market, valued in the billions, would undergo significant transformation if pig organs became widely available. Pharmaceutical companies would need to develop new immunosuppressive regimens tailored to xenotransplants. Insurance providers would have to create coverage models for these expensive, life-saving procedures. At the same time, the potential savings from reduced long-term care for patients with organ failure could offset some of these costs, presenting complex calculations for healthcare economists.
For the patient at the center of this medical breakthrough, the experience has been both harrowing and hopeful. In interviews conducted with his consent, he expressed profound gratitude for the opportunity to participate in what he called "a miracle of modern medicine." His willingness to undergo this experimental procedure, despite the risks, exemplifies the courage of patients who participate in groundbreaking medical research. His ongoing recovery serves as a living testament to the dedication of the scientists, surgeons, and medical professionals who made this achievement possible.
The story of the first successful genetically modified pig heart transplant will undoubtedly be remembered as a watershed moment in medical history. Like the first human heart transplant in 1967 or the first successful kidney transplant in 1954, this achievement pushes the boundaries of what's possible in medicine. While challenges remain before xenotransplantation becomes routine, this breakthrough offers tangible hope to the hundreds of thousands of patients worldwide awaiting life-saving organ transplants. As science continues to blur the lines between species in the service of human health, we stand at the threshold of a new chapter in our ability to conquer diseases that were once considered invariably fatal.

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025